Exploring Ketamine: A Complex Treatment for Depression
Written on
Chapter 1: Understanding Ketamine's Role in Mental Health
Ketamine is currently at the center of a heated debate. Often labeled as an addictive and potentially hazardous substance, it has been implicated in high-profile incidents, such as the overdose death of actor Matthew Perry. On the other hand, discussions led by experts like Andrew Huberman highlight its potential as a groundbreaking treatment for depression, suggesting it could revolutionize the management of severe mental health disorders.
This presents a fascinating contradiction: a substance associated with addiction that may also offer a solution to significant psychiatric challenges.
However, the reality is that the supporting evidence is not as compelling as one might hope. While some studies indicate that ketamine could benefit individuals suffering from depression, the overall data remains inconclusive.
Theoretical Framework
Numerous hypotheses exist regarding ketamine's possible benefits for conditions like depression and bipolar disorder. The predominant theory revolves around its impact on the brain. Ketamine functions as an NMDA antagonist, inhibiting receptors that respond to N-methyl-d-aspartate (NMDA), resulting in various biochemical changes that may relate to mental health issues.
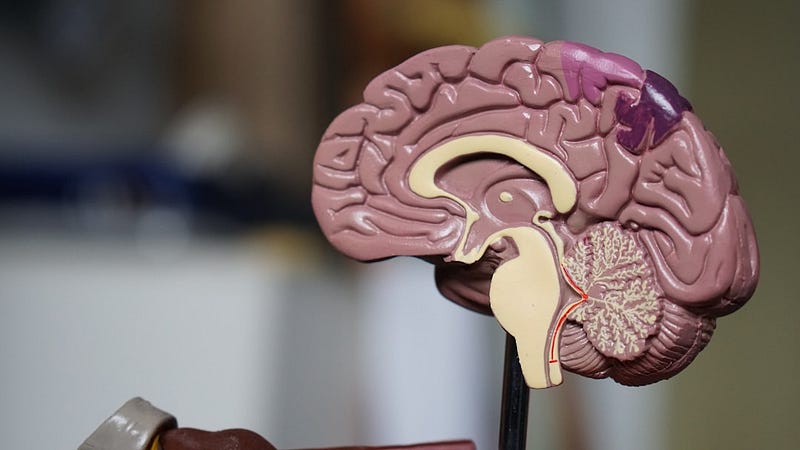
These biochemical theories are intricate and likely beyond the scope of this discussion, but they involve complex interactions between neurochemicals and how ketamine alters these interactions, potentially altering the experience of depression. For a detailed exploration, refer to the linked article that summarizes these mechanisms.
Another explanation for ketamine's antidepressant effects is simpler: the euphoric feelings it can induce. Depending on dosage, ketamine can result in effects ranging from pain relief and sedation to dissociative experiences and hallucinations. While the relationship between these experiences and mood improvement is more complicated, many believe that the combination of dissociation and altered brain chemistry might alleviate depressive symptoms.
The common thread in these theories is the consistent observation that individuals who use ketamine report significant improvements in their depressive states.
Real-World Studies
However, theories often falter under scrutiny. Our understanding of depression itself is still limited, making it challenging to formulate a comprehensive theory explaining its complexities.
This is why human studies are essential. Initial trials investigating ketamine's potential for treating depression date back to the late 1990s and early 2000s. Since then, numerous studies have examined its effectiveness in alleviating depressive symptoms.
A recent Cochrane review, which is considered a gold standard in evidence-based medicine, identified 31 randomized clinical trials that assessed ketamine's effects. The findings suggested that, within 24 hours, individuals receiving ketamine reported significantly better scores on depression-related questionnaires compared to those given placebos. A similar trend was observed with a specific ketamine variant, esketamine.
Nevertheless, there are substantial concerns regarding this analysis. The short timeframe—only 24 hours—raises questions about the sustainability of the reported benefits. While some evidence suggests that repeated doses may yield longer-lasting effects, the studies available are minimal and not robust enough for definitive conclusions.
Moreover, many studies involved small sample sizes and lacked rigorous controls. For instance, a study involving just 16 older adults in a crossover design provides little actionable insight due to its size. The Cochrane review rated the overall quality of evidence as very low, indicating that the studies were not sufficiently reliable to draw meaningful conclusions.
A critical issue arises from the inability to blind participants effectively. Most individuals receiving ketamine are likely to recognize they are on the drug due to its hallucinatory and sedative effects. Consequently, trials often depend on self-reported outcomes, meaning that while individuals may feel an improvement in their mental health, it remains uncertain whether this is due to ketamine itself.

One notable blinded trial, albeit controversial, randomized individuals undergoing anesthesia to receive either a ketamine infusion or a saline placebo. Upon waking, participants were unaware of which treatment they had received, and this study reported no mental health benefits from ketamine compared to saline.
While this trial is significant, it included only 40 participants, and the short duration and design limitations weaken its conclusions. Nonetheless, it suggests that much of the positive feedback from other studies could stem from participants' expectations rather than the drug's actual effectiveness.
Conclusion
Despite the seemingly skeptical tone, I maintain a cautiously optimistic view on ketamine's potential in mental health treatment. It is one of several pharmaceutical options that may be undervalued due to misuse in other contexts, akin to substances like psilocybin or MDMA.
That said, the exuberance often expressed within certain communities appears largely unfounded. While there is a chance that ketamine holds significant untapped potential for treating depression, current evidence is mixed and far from conclusive.
The key takeaway is the pressing need for more comprehensive and rigorous research. Collating numerous small studies may lead to misleading conclusions. The Cochrane review is particularly disheartening, as none of the trials demonstrated a strong, convincing benefit, primarily due to their small scale.
The most extensive study conducted to date was released in 2023 and involved two phases: one with a fixed dose of ketamine or a benzodiazepine called midazolam, and another allowing dosage adjustment. Initially, no benefits were observed with ketamine, but the second phase revealed substantial improvements. However, the blinding issues in both phases raised questions about the validity of the findings.
I remain hopeful about ketamine's potential benefits for mental health. However, it is crucial to approach such claims with caution until more definitive studies are conducted to clarify its efficacy in treating depression and related disorders.
The first video titled "Ketamine & Depression: How it Works - Yale Medicine Explains" provides a comprehensive overview of the mechanisms behind ketamine's effects on depression.
The second video titled "Ketamine as a Treatment for Depression?" delves into the ongoing debates and findings regarding ketamine's therapeutic potential.