Sleep Patterns as Potential Early Indicators of Alzheimer’s Disease
Written on
Chapter 1: Understanding Alzheimer’s Disease
Alzheimer's disease (AD) is a progressive neurodegenerative condition impacting millions globally. Dementia, in general, affects over 55 million individuals, with approximately 60 to 70% diagnosed with Alzheimer’s. Each year, an additional 10 million people are added to these statistics. However, these figures may be conservative, as emerging research suggests a higher prevalence.
The search for effective treatments has been arduous. Commonly referenced are amyloid plaques found between neurons and neurofibrillary tangles within them. Nonetheless, numerous other issues arise in the brains of those with Alzheimer's: the blood-brain barrier deteriorates, oxidative stress increases, mitochondrial dysfunction occurs, and inflammation becomes widespread.
A significant issue is that diagnoses often occur too late. The question remains: can we foresee the onset of Alzheimer’s? While scientists are investigating specific blood proteins and ocular changes as potential predictive markers, advancements in machine learning may also help diagnose early dementia via MRI scans.
Moreover, a closer examination of sleep patterns may offer insights.
Section 1.1: Sleep Waves and Their Implications
During sleep, the brain exhibits rhythmic activity patterns, which are essential for memory consolidation and cognitive function. These brain waves include phenomena known as theta bursts, sleep spindles, and slow waves.
Recent studies indicate that these sleep wave patterns could serve as a biomarker for the early detection of Alzheimer’s disease. Researchers engaged 205 participants, either cognitively unimpaired or mildly impaired, in a series of assessments. These included single-channel EEG recordings, home sleep apnea tests, APOE4 genotyping, lumbar punctures for Alzheimer’s biomarkers, and Clinical Dementia Rating (CDR) evaluations. Participants were monitored over several nights using a forehead-mounted single-channel EEG device.
The findings revealed that specific types of slow-wave sleep (SWS) oscillatory events, particularly those with high and low transition frequency subtypes, are linked to memory performance. Notably, significant variations in SWS-coupled theta burst power were observed among cognitively impaired individuals, implying that alterations in SWS may signal early signs of Alzheimer’s disease.
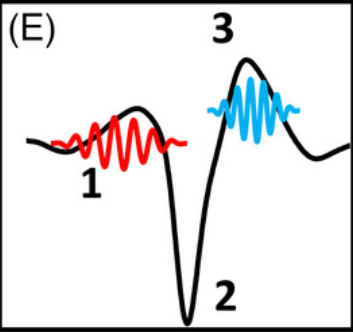
Illustratively, examining an EEG of sleep activity shows three components: 1 represents the theta burst, 2 denotes the slow wave, and 3 illustrates the sleep spindle.
Cognitive impairment leads to observable changes: in one scenario, reduced theta burst power is evident, and as researchers identify known Alzheimer’s biomarkers in cerebrospinal fluid, these changes are reflected on the EEG.
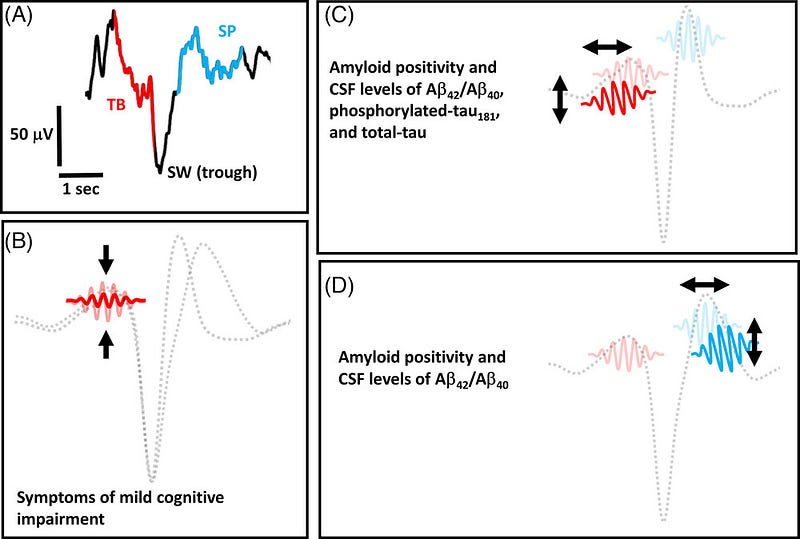
(All illustrations from Pulver et al. 2023 Mapping sleep’s oscillatory events as a biomarker of Alzheimer’s disease. Alzheimer’s & Dementia. doi: 10.1002/alz.13420)
These findings hold considerable promise for the future of Alzheimer’s diagnosis and treatment. Currently, cognitive assessments and brain imaging are the standard diagnostic methods, both of which can be costly and invasive. This research suggests that monitoring sleep patterns may provide a non-invasive and more affordable approach to identifying early signs of Alzheimer’s disease.
The authors project that recognizing oscillatory events during sleep could have clinical applications as indicators of brain health and early detection of neurodegenerative processes. This technique merely requires a single-channel EEG in a home setting, paving the way for affordable, user-friendly EEG “wearable” headbands to monitor brain health, assess neurodegenerative disease risk, and evaluate treatment responses.
However, the authors also recognize certain limitations. The study's sample size was relatively small, and participants were predominantly white and well-educated. Further investigation is necessary to examine the link between sleep patterns and Alzheimer’s in a larger, more diverse cohort.
Additionally, the study did not explore the causal relationship between sleep disturbances and Alzheimer’s disease. It remains unclear whether sleep issues are a risk factor or a symptom of the disease.
Despite these limitations, it appears that mapping the oscillatory events of sleep could emerge as a valuable biomarker for early Alzheimer’s detection.
Night, night.
Chapter 2: Exploring the Connection Between Sleep and Alzheimer’s
This video discusses the relationship between sleep, cognition, and Alzheimer's disease risk, highlighting how sleep disturbances may influence cognitive decline.
In this video, experts outline the early signs of Alzheimer’s disease, emphasizing the importance of recognizing symptoms for timely intervention.